Celebrex®
Featured Content
Safety & Tolerability

CELEBREX® demonstrated a lower incidence of clinically significant GI AEs1,2
Mode of Action
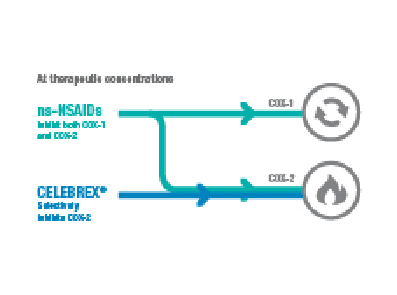
Celebrex® is an (NSAID) with anti-inflammatory, analgesic, and antipyretic activities1
CELEBREX® demonstrated a lower incidence of clinically significant GI AEs1,2
Celebrex® is an (NSAID) with anti-inflammatory, analgesic, and antipyretic activities1